메가슬롯
슬롯을 위한 아시아의 가장 큰 전문 사이트!
신규 가입 20% 보너스 + 1만 쿠폰 지급!
올인 마지막 입금액의 10% 쿠폰
레벨별 콤프 0.1%~0.6% 가입 동시 적립!
메가슬롯 홈페이지

페이지 최상단의 배너나 바로가기를 통해 메가슬롯 공식 홈페이지로 넘어갑니다.
현재 제공하는 이벤트들을 한눈에 보고 싶으시다면, 홈페이지 좌측 상단의 이벤트안내 탭을 눌러주세요.
이외 모든 기능, 실시간 잭팟금액 조회, 입출금 신청, 쿠폰 발급 현황 파악, 머니 이동 기능까지 포함하여 이용 가능합니다.
홈페이지의 맨 아래에 위치한 텔레그램과 위쳇 고객센터 정보를 이용해, 서비스 사용 중에 생기는 문제를 해당 경로로 문의하실 수 있습니다.
메가슬롯 주소 게임 목록
공식 홈페이지 하단에 40개 이상의 다양한 슬롯 게임사 목록이 제공됩니다. 아래 내용은 메가슬롯에서 정식 계약을 맺고 제공하는 정품 슬롯 게임사 리스트입니다.
- 마이크로
- 드래곤소프트
- 와즈단
- 릴렉스
- 레드레이크
- 후가소
- 스피어헤드
- 아리스토클랏
- 스피어헤드
- 드래곤소프트
- 핵소게이밍
- 프라그마틱
- 키론
- 릴렉스
- 썬더킥
- 1X2게이밍
- 마이크로
- 게임피시 글로벌
- 아이언독
- 프라그마틱
- 리얼타임게이밍
- 스피어헤드
- 우후게임즈
- 모빌랏
- 아이언독
- 모빌랏
- 이엘케이
- 와즈단
- 에보플레이
- 1X2게이밍
- 후가소
- 분고
- 드래곤소프트
- 스프리트락
- 플레이앤고
- 플레이앤고
메가슬롯 조작 이벤트
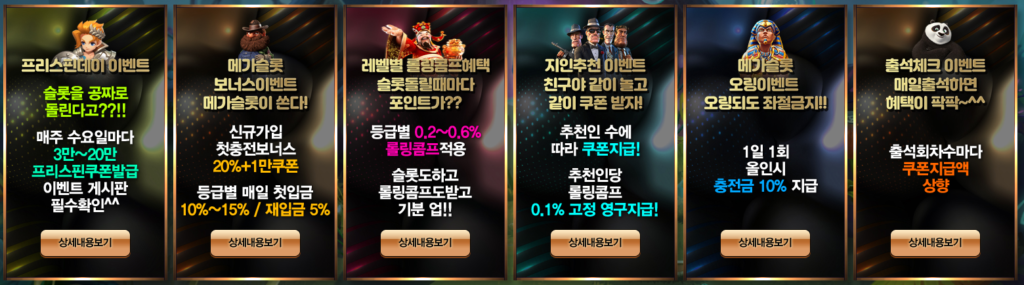
프리스핀데이 이벤트
매주 수요일, 메가 프리스핀 데이 이벤트가 개최됩니다
- 매주 수요일 활동내역별 프리스핀데이 쿠폰지급(해당 주 월요일, 화요일 활동내역)
- 고객센터 채팅창으로 이벤트 신청 후 이용할 게임 확인 / 본사에서 정한 슬롯게임만 이용 가능
- 프리스핀 쿠폰은 수요일 하루만 사용 가능
- 최대 출금 3배, 롤링 3배
- 프리스핀 쿠폰은 절대 입금액과 동시에 사용 금지, 사용 시 전액 몰수 처리
메가슬롯 신규가입 이벤트
신규 가입 시 메가슬롯에서는 첫 충전에 대해 아래와 같은 보너스를 제공합니다.
신규가입 첫충전 보너스 20% + 1만 쿠폰(최대 100만)
가입 후 1회 입금 20%, 2회 10%, 3회 5% 보너스 지급
매일 첫입금 보너스 10%(최대 100만)
매일 재입금 보너스 5%(최대 100만)
레벨별 롤링콤프
등급 / 롤링콤프 / 조건 / 첫충보너스
- 레드 / 0.1% / 가입시 적용 / 신규첫충 20% 이후 10%
- 실버 / 0.1% / 누적충전 1천만원 이상 / 첫충 10%
- 골드 / 0.2% / 누적충전 1억원 이상 / 첫충 10%
- 플래티눔 / 0.25% / 누적충전 4억원 이상 / 첫충 10%
- 에메랄드 / 0.3% / 누적충전 8억원 이상 / 첫충 11%
- 루비 / 0.4% / 누적충전 15억원 이상 / 첫충 12%
- VIP / 0.5% / 누적충전 25억원 이상 / 첫충 15%
- VVIP / 0.6% / 누적충전 60억원 이상 / 첫충 15%
첫충 보너스 최대 100만
매주 일요일, 만 원 이상 금액에 한해 천 원 단위로 콤프를 사용할 수 있습니다.
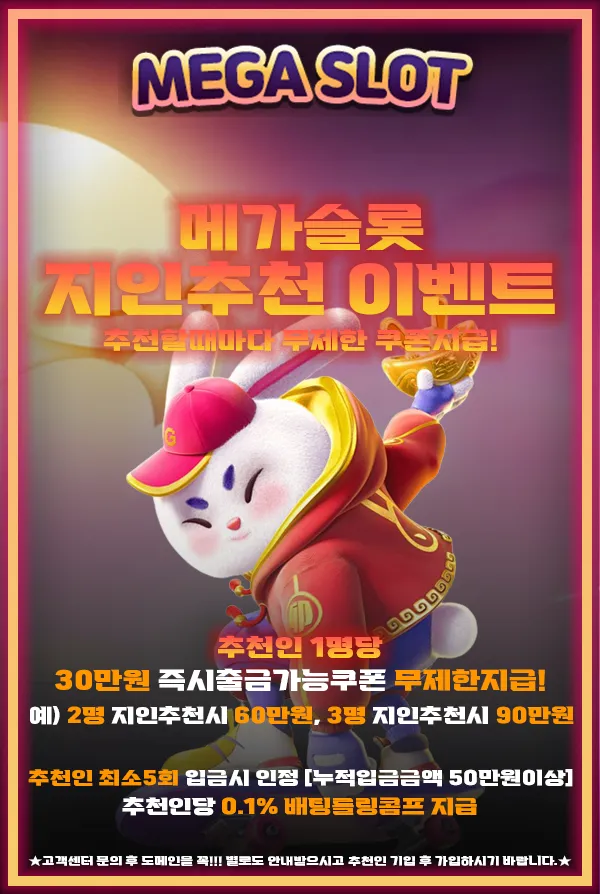
메가슬롯 지인추천 이벤트
추천인 수에 따라 아래와 같이 쿠폰 지급
- 추천인 3명 – 6만원 쿠폰
- 추천인 5명 – 10만원 쿠폰
- 추천인 10명 – 20만원 쿠폰
누적 입금액 50만 원 이상과 최소 세 번의 입금이 이루어질 경우, 한 명이 추천인으로 인정되는 조건입니다
추천인당 0.1% 배팅롤링콤프 영구 적용!
[주의사항]
- 매주 수요일 마다 1:1 문의로 추천인 쿠폰 요청시 발급
- 다수의 계정 사용이나 같은 IP 주소 사용이 발견될 경우, 자금을 몰수합니다
- 쿠폰만 사용 시 롤링 300%, 최대출금 3배까지 지급
- 이벤트 및 보너스 악용 회원은 게임 이용 제재
- 이벤트 기간 동안 이벤트 내용은 변경될 수 있습니다.
텔레그램 공식채널 이벤트
메가슬롯 공식채널에 참여한 모든 회원들에게 2만 쿠폰 지급!
신속한 공지와 정보를 위해, 공식 채널 참여를 적극 권장합니다.
[이벤트 참여 방법]
- 고객센터를 통해 공식채널 링크 문의
- 공식채널 입장 후 고객센터로 스크린샷 첨부
- 채널 이벤트 2만 쿠폰 확인

무료 메가슬롯 머신 : 모두의슬롯
온라인 슬롯 게임의 세계로 떠나 스릴 넘치는 여정을 시작할 준비가 되셨나요? 메가슬롯은 거대한 보상을 약속하며 여러분을 기다립니다! 고품질 그래픽, 혁신적인 기능, 그리고 흥미진진한 게임 경험을 즐겨보세요.
다양한 주제와 흥미로운 보너스 라운드로 모든 스핀은 기대와 잠재적인 부를 가득 담고 있습니다. 클래식한 과일 슬롯을 선호하든, 현대적인 비디오 슬롯을 즐기든, 누구나를 위한 무언가가 있습니다. 이미 이 흥미로운 경험을 한 전 세계의 다른 플레이어들과 함께하세요. 대담한 사람들에게 유리한 아드레날린으로 넘치는 세계를 경험하세요.
메가슬롯을 플레이하는 것은 현재의 큰 보상을 얻을 수 있는 흥미로운 기회를 제공하는 아주 즐거운 경험입니다. 먼저 원하는 기기에서 손쉽게 게임을 시작하세요. 목표는 릴 전체에서 일치하는 기호를 사용하여 승리 조합을 만드는 것입니다. 이를 위해 게임의 작동 방식을 이해해야 할 것입니다. 일반적으로 다섯 개의 릴과 여러 개의 페이라인 또는 승리 방법으로 구성됩니다.
메가슬롯 게임 | 슬롯 가입쿠폰, 지금 당신의 것으로 얻으세요!

릴을 회전하기 전에 베팅 크기를 기호에 따라 조절합니다. 그런 다음 스핀 버튼을 누르고 기호가 무작위로 나타나는 것을 확인합니다. 와일드나 산점과 같은 특별한 기호를 주시하고, 자유 스핀이나 미니 게임과 같은 흥미로운 보너스 기능을 활성화할 수 있습니다. 일부 메가슬롯은 무작위로 또는 특정 기호 조합으로 얻을 수 있는 점진적인 잭팟도 제공합니다.
메가슬롯의 세계에서 플레이어들은 릴이 돌아가는 흥미 뿐만 아니라 엄청난 보상의 약속으로 인생을 현실로 바꿀 수 있는 기회를 얻습니다. 캐시 잭팟부터 이국적인 여행지에서의 호화로운 휴가까지 다양한 수익성 있는 보상이 플레이어들을 기다립니다.
초보자든 숙련된 플레이어든 간에, 항상 놀라운 것이 있습니다. 하지만 그것은 단지 큰 승리에 관한 것이 아닙니다 – 그것은 모든 플레이어가 보상을 받을 수 있는 기회를 보장합니다. 다양한 보너스 기능과 게임 플레이에 포함된 미니 게임으로, 더 작은 승리도 합쳐지고 아주 신나는 경험을 만들 수 있습니다. 그러므로, 다른 어떤 것들과 같은 모험을 준비하세요.
투데이슬롯
게임의 부드러운 운용은 사용자가 액션에 깊이 몰입하게 만드는 매혹적인 경험을 제공합니다. 눈길을 끄는 비주얼과 매력적인 애니메이션은 게임의 각 순간을 생동감 있게 만들어 전체적인 플레이 품질을 높여줍니다. 다양한 보너스 라운드와 무료 스핀 기능을 통해 큰 이익을 얻을 수 있는 기회가 늘어납니다.
메가슬롯 게임은 다양한 특별 기능과 보너스 라운드를 제공하여 플레이어에게 스릴 넘치는 게임 경험을 선사하며, 이를 통해 승리할 기회를 더 많이 제공합니다. 와일드 기호는 눈에 띄는 기능으로, 다른 기호들을 대체할 수 있는 뚜렷한 로고로 표현되어, 승리 조합을 이룰 가능성을 향상시킵니다. 또한, 스캐터 기호는 게임을 한층 더 흥미롭게 만드는 보너스 라운드를 활성화시킬 수 있습니다.
메가슬롯 게임에 포함된 프리 스핀 기능은 스릴 넘치는 추가적인 특징으로, 스캐터 기호 3개를 모으면 무료로 스핀할 수 있는 기회가 주어지고, 해당 기간 동안 이루어지는 모든 승리는 배가 됩니다. 이는 추가적인 비용 부담 없이 큰 이득을 얻을 수 있는 좋은 기회며, 또한 보너스 라운드에서는 독창적인 미니 게임이 등장합니다. 이 게임들은 플레이어의 승리 가능성을 최대화하기 위해 전략적 사고를 필요로 합니다.
메가슬롯 후기 FAQ 자주 묻는 질문
메가슬롯에서 다른 카지노나 스포츠 베팅도 지원하나요?
아니오, 메가슬롯은 슬롯 게임 전용 사이트로서, 오직 정품 게임만을 취급합니다. 이는 슬롯 게임에서의 퀄리티를 양과 질 모두에서 보장합니다.
메가슬롯 궁금한 점이나 문제가 생겼을 때 어디에 문의하면 되나요?
언제든지 공식 웹사이트 하단에 소개된 고객센터 계정으로 문의를 주시면, 24시간 내로 신속하게 대응해드립니다. 텔레그램 공식 채널의 가입 이벤트도 이용해 추가 혜택을 받으실 수 있습니다.

